The Medicare program last year implemented a pilot program in three states, including South Carolina, in response to the increased use of nonemergency ambulance transports between 2002 until 2011. Private ambulance company owners in South Carolina have become increasingly critical of Medicare’s experiment to eliminate fraud and save the federal government money. There are plans to expand this program to five other states in 2016.
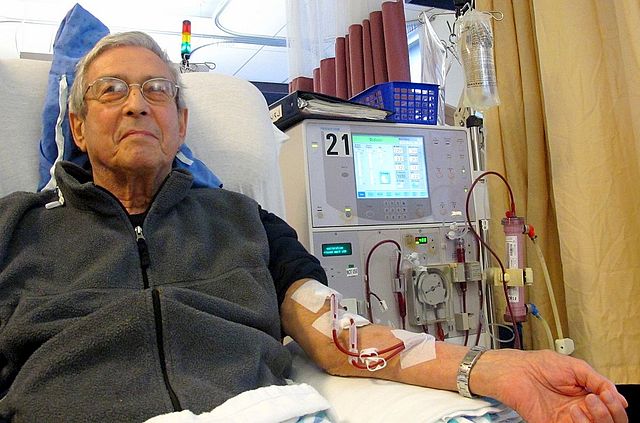
The new federal pilot program is leaving some patients with debilitating illnesses unable to get the transport they need for life saving treatments. The rides are covered by Medicare for those who need medical attention on the way to dialysis or chemotherapy treatments. “They give me a service that is absolutely necessary,” according to Dick Linder, who takes an ambulance on a regular basis for dialysis treatment.
Ambulance companies have found in the first year of the pilot program in South Carolina, that the Medicare contractor, Palmetto GBA has made inconsistent decisions about payment for the nonemergency transports to treatment. The CEO of Medtrust, Josh Watts, says the federal pilot program to expand prior authorization for repetitive nonemergency transports will cost patients their lives, and the increasing amount of paperwork to file a claim is putting ambulance companies out of business.
“Most of us got into the business to help people, and what that means is we will over extend without the ability to bill,” he explained.
The Department of Health and Human Services began the pilot program in response to the escalating use of nonemergency transports between 2002 and 2011. Hospital rides rose by 55 percent, trips to dialysis treatments skyrocketed by 269 percent, and transports for mental health services jumped up 829 percent during this time period.
Local news station Channel 2 News I-Team did a recent story on this issue, but the Medicare carrier, Palmetto GBA, declined to be interviewed. They released a statement which said:
“Palmetto GBA is consistent in the application of the Center for Medicare and Medicaid Services (CMS) guidelines. Our oversight ensures that taxpayer dollars are spent appropriately for the services it covers. It should be noted that the long-standing Medicare guidelines for ambulance transport have not changed at all. Prior authorization did not create a new clinical documentation requirement. Instead, it requires the same information necessary to support Medicare payment—just earlier in the process. It actually helps the patient to have the documentation submitted up front, which ensures that if there are questions, they get addressed early on.”
Prior authorization is required every 60 days and takes up to 20 business days to be approved by Medicare. “Taking a patient that we have gotten through the gauntlet and they’ve been approved, 60 days later, we have to do that process again,” Watts said. “For a patient that has no legs, has no arms, and is blind, they aren’t getting better.”
Medtrust Medical Transport provides emergent and non-emergent ambulance services in Charleston, Myrtle Beach, and Georgetown, SC.